New drug is not the answer for breast cancer patients, earlier screening is - Claire Strachan
‘Anastrozole’ is hailed as great news, potentially preventing 2,000 cases of breast cancer and saving the NHS around £15m in treatment costs.
Diagnosed with breast cancer myself over a year ago, I have been through the system and have now been taking Anastrozole for about eight months, and I’ve been told to take it for 10 years. Out of a number of friends also offered the medication post-surgery, I am the only one who has been able to continue taking it as one of the biggest side effects is anxiety and depression.
Advertisement
Hide AdAdvertisement
Hide AdThe best description I could give is waking up feeling like the room is filled with dementors and them then following you round all day.

Hearing the words, ‘you are right you have cancer’ is one of the hardest things I think I have been through.
I was actually on holiday when I saw an indentation in the mirror, and thanks to a friend regularly sharing a grid of symptoms to look out for, I did realise the moment I saw it that it was probably cancer, and I then found the lump. My surgeon credits the mirror for saving my life.
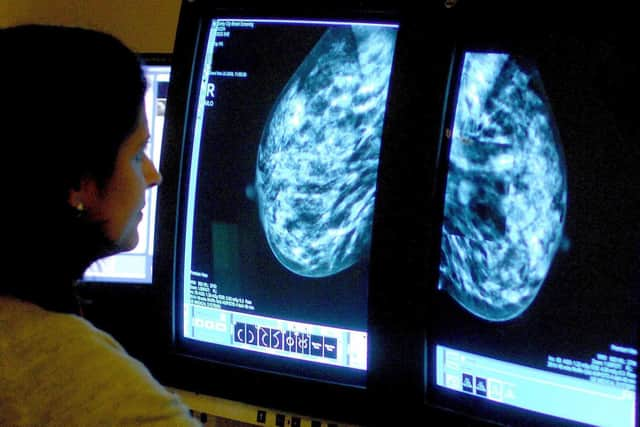
Aged 50 at the time, I had not received a letter for my first offer of screening and a mammogram. That letter arrived six months after my diagnosis and was clearly too late. From friends also diagnosed before their first screening, I think the age should be brought back to 45.
Advertisement
Hide AdAdvertisement
Hide AdTaking tablets is just one solution, but as they result in then taking more tablets to counteract the impact, isn’t offering earlier screening a better solution? I was horrified to see NHS stats that only 50 per cent of women take up the offer of their first screening, but even if 50 per cent did at an earlier age, surely that would be a much more effective preventative measure?
Having previously been treated for Long Covid, under care at the Harrogate Covid Clinic, St Barts in London and the Manchester Cough Clinic – they too took a similar approach. Unable to lose the Covid cough, the end solution was medication and to put me on morphine for the rest of my life, which I declined. Instead I used acupuncture and complementary therapies, and they cured the damage to my vagus nerve. The only consultants interested in the result were at St Barts, Manchester who suggested the morphine simply discharged me from the clinic.
It has also been a rollercoaster ride in terms of the comparison between private healthcare and the NHS. I was fortunate enough to have private healthcare, or so I thought, but in addition to dealing with a cancer diagnosis, I also had to battle with incredibly poor customer service through Bupa.
One year on I have finally had the all clear for now, which is a weight off my shoulders, but change is needed, both relating to education and diagnosis. The screening age is a priority in terms of needing to be made earlier. It is great that medication exists to help prevent the disease, but certainly the impact of anyone I know who has taken it, is that it will only result in the need for additional medication, which is another cost again to the NHS.
Claire Strachan is a marketing, PR and fundraising consultant.
Comment Guidelines
National World encourages reader discussion on our stories. User feedback, insights and back-and-forth exchanges add a rich layer of context to reporting. Please review our Community Guidelines before commenting.